This brochure contains general information for donors whose blood stem cells will be harvested from their blood. The brochure also contains background information on blood stem cell transplantations.
Wherever stem cells are mentioned in this brochure, they refer to blood stem cells; wherever stem cell transplantation is mentioned, it refers to blood stem cell transplantation.
We trust this information will give you a proper understanding of what it means to b a donor. Should you have any questions after reading this brochure, please feel free to ask the medical examiner, physician assistant (PA) or the stem cell transplantation nurse (SCT nurse).
This brochure contains various technical terms, the most common of which are explained in the final chapter of this brochure.
What is allogeneic stem cell transplantation?
The best treatment option for a number of blood and bone marrow diseases, such as aplastic anemia, leukemia, non-Hodgkin’s lymphoma, multiple myeloma and myelodysplasia, is allogeneic stem cell transplantation. When treated with an allogeneic stem cell transplant, the patient receives stem cells from a donor.
Prior to undergoing the allogeneic stem cell transplantation the patient is treated with cytostatics, sometimes in combination with total body irradiation. This treatment is intended to reduce the number of cancer cells, but especially to lower the patient’s immune system, so that the donor’s stem cells will be accepted.
After the cytostatics are administered, whether or not in combination with total body irradiation, the donor stem cells are delivered to the patient via an infusion. The donor stem cells themselves seek out the patient’s bone marrow cavity. They will settle there and start producing new blood cells about 2 to 3 weeks later.
The donor’s immune cells (T-lymphocytes) that are contained in the transplant and that originate from the stem cells, are able to combat any remnant cancer cells in the patient. However, they can also recognize normal body cells as alien cells. The latter can lead to the ‘graft-versus-host’ disease. (This is a kind of rejection; you can read more about this in Chapter 10).
What is blood and bone marrow?
Blood is a fluid that circulates in the body for the distribution of nutrients and oxygen and the disposal of waste. Blood is formed in bone marrow. Bone marrow is located in the bones. Stem cells live in the bone marrow.
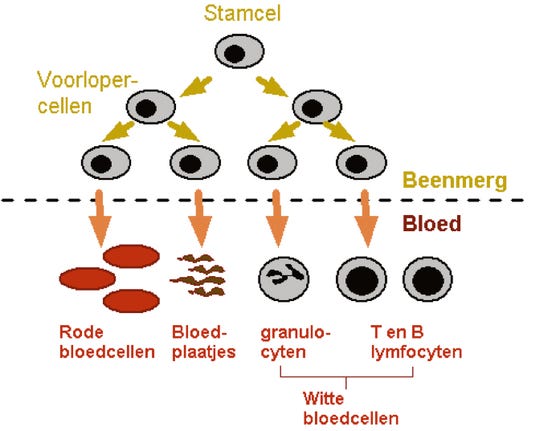
These stem cells divide and mature into red and white blood cells and platelets. Many millions of cells are produced each and every day to keep the number of blood cells up. Mature blood cells leave the bone marrow and enter the bloodstream.
Blood consists not only of blood cells but also of plasma. Plasma is mainly composed of water, proteins, nutrients, vitamins, hormones and salts. Approximately 5 liters of blood circulate in an adult body.
Below is a simple diagram of blood production: from stem cell to mature cell.
What is the function of blood cells?
Three groups of blood cells are distinguished in the blood:
1 The red blood cells (erythrocytes) carry oxygen from the lungs to the tissues. A lack of red blood cells is called anemia. Tissue markers on the red blood cells determine the so-called ABO blood group.
2 The white blood cells (leukocytes) are responsible for the immune system. There are various types of white blood cells.
a.The granulocytes help fight off bacteria.
b. The lymphocytes help fight off viruses. Tissue markers on the lymphocytes determine the HLA groups.
T-lymphocytes can kill foreign cells. They are responsible for the disease-fighting activity of the donor transplant, but also for the graft-versus-host disease.
3 The platelets (thrombocytes) play an important part in blood coagulation (clotting).
Stem cell donation
When stem cell transplantation is considered a good treatment option for a patient, a donor is sought.
Tissue typing or HLA typing
Tissue typing (HLA typing) is needed to determine whether you could be a suitable donor; this is followed by an examination for a match with your sibling. The HLA on the white blood cells can be determined by taking a blood sample. HLA stands for Human Leukocyte Antigen. It takes approximately 4 to 6 weeks after the blood sample is taken to know whether you are a suitable donor. If the tissue typing is a match, the SCT nurse will phone you. If your tissue typing is not a match with that of your sibling, you will receive the result in writing.
What exactly does HLA typing mean?
HLA (Human Leukocyte Antigen) is a code for markers on body cells. Those markers tell the body whether the body cells match with your body. Immune responses occur when the HLA typing of certain cells does not match. Tissue typing is needed to determine whether you are a suitable donor for your sibling.
We examine whether your tissue type and your sibling’s tissue type match up on 10 points. If the tissue type does not match, there is a greater risk that the transplanted cells will be rejected. The HLA type is hereditary. One half is inherited from the mother, the other half from the father. The chance that two children from the same parents have an identical combination is one in four, 25%. The information (the genes) for the tissue type is on a different chromosome, than, for example, the genes for the sex or ABO blood group. So you, as a donor, do not have to be of the same sex as the patient nor have the same blood type. If there are several suitable donors, the choice of donor is made on the basis of the HLA type, virus markers in the blood, sex, age and health status of the donors.
A parent is hardly ever an identical donor for a child, only semi-identical. Of all 23 chromosome pairs, one chromosome is from the mother and one from the father. As a result, one chromosome is always identical, but the other is different. Should stem cell transplantation with a semi-identical donor be considered a good treatment option in the future, we will inform you accordingly.
Criteria for stem cell donation
There are a number of criteria that you, as a donor, must meet:
- You must have an identical tissue type (HLA type).
- You must be in good health in order to be able to endure the harvest procedure.
- You may not carry any diseases that are transmitted via the blood and that may be detrimental to the recipient.
- Your own blood production in the bone marrow must be normal.
- You may not be pregnant.
Anyone who has or has had any of the following conditions in the past, CANNOT be a donor:
- A malignant disease (a type of cancer) with the exception of locally treated basal cell carcinoma of the skin;
- Hemophilia, von Willebrand’s disease, sickle cell disease or beta thalassamia;
- CVA or TIA;
- Systemic autoimmune diseases (such as rheumatism, celiac disease, Crohn’s disease);
- Single organ diseases (such as severe liver, kidney or lung problems);
- Uveitis;
- An epileptic seizure that occurred less than a year ago;
- HIV or AIDS;
- Severe obesity (Body Mass Index 40 or higher).
HLA typing results
The SCT nurse will notify you if the blood tests show that the HLA type is a match. You then have 24 hours to reflect and decide whether you are willing to undergo the donation process. During these 24 hours your sibling will not be informed about your suitability as a donor. You have the option to anonymously reject being a stem cell donor. The SCT nurse will contact you again 24 hours later. If you are still willing to being a stem cell donor the patient will be informed that you are suitable as a donor.
Motivation
Stem cell donation occurs on a voluntary basis. Donating stem cells for a brother or sister can be a matter-of-course. There are, however, situations where it is not. The reasons why you cannot or do not want to be a donor are not discussed with the patient. The patient’s attending physician will be informed that there is no suitable donor. Your privacy is protected to the very best of our ability. Should you have doubts about being a donor please contact the SCT nurse.
Even at a later stage you can still have doubts about becoming a donor, in which case we advise you to contact the SCT nurse. Withdrawing your consent can have major consequences for the treatment and the course of the patient’s illness.
Donor examination
Appointments
If you are willing to be a donor, you will be called up for a medical examination and information session. If possible, the appointments will be planned for the same day. You will receive a letter with the following appointments:
- With the laboratory for a blood sample: A total of five or six 5-10 ml vials of blood are taken. The blood test is to check whether you have enough blood cells, whether there are no abnormal cells in your blood and whether your liver and kidneys function properly. It also checks whether you are (or have been) infected with certain viruses, such as hepatitis B+C, herpes viruses, cytomegalo- virus, (CMV), Epstein-Barr virus (EBV) and HIV, the virus that causes AIDS.
- With the Cardiology department: For an electrocardiogram (ECG).
- With the SCT nurse: For making your acquaintance and for providing information about the donor track and the stem cell apheresis.
- With the medical examiner/physician assistant (PA): For the medical examination, during which your blood test results are discussed, questions are asked pertaining to your health and a physical examination is performed.
The medical doctor/PA will contact you by phone one week after the medical examination to discuss the results of the examination. If a result of an examination differs from the norm, follow-up examinations might be required or you might be turned down as a stem cell donor.
Your general practitioner will be informed of the result of the medical examination.
Three to four weeks before the stem cell donation you will have an appointment:
- With the laboratory for a blood sample to test for viruses (this result is valid for a maximum of 30 days);
- For women, possibly a pregnancy test;
- With the SCT nurse for injection instructions and to receive the growth factor
Informed Consent
If you agree to being a donor, we will ask you to sign an informed consent form. This is a written statement in which you state that you have been informed about the procedure and in which you give your permission for the anonymous use of your data. You will receive the informed consent from along with the invitation for your first visit to the nurse and the medical doctor/PA. You can ask any questions you might have about this form during your first visit.
The informed consent includes a declaration of consent for the donation of bone marrow. Sometimes the stem cells cannot be harvested from the peripheral blood, in which case several bone marrow punctures must be performed under an anesthetic so as to obtain bone marrow (containing the stem cells).
Both you and the medical examiner/PA are required to sign two informed consent forms. One copy for yourself and one copy for in the medical status file.
Harvesting stem cells
Stimulating stem cells
Basically, the stem cells are taken from your blood. By nature, stem cells occur only in small numbers in the bloodstream. To be able to harvest stem cells, the bloodstream must contain a large number of stem cells. With the aid of a growth factor the stem cells are stimulated to migrate to the bloodstream.
Growth factors are molecules that are produced by the body itself. They stimulate the production of blood cells in the bone marrow. Under the influence of the G-CSF (Filgrastim®) growth factor the number of stem cells in the bone marrow increases and stem cells migrate (mobilize) to your blood. The growth factor is available as a medicine in injection fluid.
Administering injections with growth factor
The G-CSF injection fluid is administered as an injection under the skin (subcutaneous injection). It can be injected in a skin fold in the abdomen or in the upper leg. It is a simple procedure that you, your partner or relative can learn. The SCT nurse will instruct you (or your partner/relative) on how to administer the injection. Two subcutaneous injections of G-CSF (Filgrastim, Neupogen®) per day, for 5 days, are usually enough to get sufficient stem cells into the bloodstream. On the fifth day, after nine G-CSF injections have been administered, the harvesting of the stem cells can commence.
The SCT nurse will give you the syringes, a needle container and an administration schedule to take home with you. The syringes containing G-CSF are ready for use and must be stored in the refrigerator (at 2-8 degrees Celsius). The expiry date is stated on the packaging.
Note: Syringes that are unintentionally stored outside the refrigerator will keep for 7 days, provided they are not cloudy.
Side effects of the injections with growth factors
The G-CSF injections can cause pressure on the bone membranes, with bone pain as a consequence. This bone pain is often felt in the back, on the sternum (breastbone) or in the cranium (skull); the amount of pain varies from mild to acute. Paracetamol is usually an effective painkiller for reducing the symptoms (maximum use 1 gram 4 times a day). You might also suffer flu-like symptoms, headaches, muscular pain or nausea. As soon as the G-CSF is no longer administered, the complaints will quickly disappear.
The G-CSF injection (Filgrastim/Neupogen) has been available since 2001 for donors as a medicine, during which time it has been proven to be safe. Should you have any questions regarding symptoms or anxiety on the days that you inject G-CSF or after the stem cell apheresis, we advise you to contact us by telephone. Phone numbers are listed at the end.
Harvesting stem cells
The stem cells in the blood are harvested with an apheresis machine. We call this procedure a stem cell apheresis. A stem cell apheresis takes four to six hours on average. Sometimes it is necessary to repeat this procedure the following day if not enough stem cells were harvested the first time around. In that case, you must inject G-CSF again on the evening of the fifth day and the morning of the sixth day. The nurse will give you two more syringes. You return home and the procedure is repeated the next morning.
The picture below shows the apheresis machine as used in the UMC Utrecht.

The stem cell apheresis
What is the procedure?
On the day of the stem cell apheresis you are expected in the Hematology department, location B2 East, at 8:15 am. You report to the secretaries of the Hematology clinic (clinical secretariat, room B02.221).
Prior to the stem cell apheresis a needle is inserted in a blood vessel in both arms. Blood is drained from one arm into the machine, which then harvests the stem cells. The rest of the blood is returned via the other arm. A fairly large needle is needed given the high rate at which the blood has to flow through the apheresis machine. The needles are usually inserted in a vein in the fold of the elbow.
Inserting these needles is fleetingly painful. These needles do not allow you to move your arms during the stem cell apheresis. Sometimes a needle in one arm is inserted in a vein other than in the fold of the elbow. That will give you more freedom of movement.

You lie on a bed during the stem cell apheresis. Because you are connected to the apheresis machine via intravenous infusion lines, you cannot leave your bed during the procedure. Nor can you visit the lavatory. Needless to say, you can use a bedpan or a urinal. A blood bank employee is present during the entire procedure to operate the machine and help you with food and beverages. The apheresis physician will visit you during the stem cell apheresis.
Of course, a family member or relative may also be present during the procedure. After the harvesting procedure, a blood sample is taken to check your blood count. The infusion lines are disconnected and one needle is removed. The harvested stem cells are counted in the stem cell laboratory. If there are sufficient stem cells and your blood count is in order, the second needle is removed and you can go home. We advise you not to drive home yourself.
How does a stem cell apheresis work?
The blood is separated into different cell layers by means of a centrifuge (centrifugal force). The cell layer in which the stem cells and lymphocytes are located is extracted from the blood by the apheresis machine and collected in a bag. This requires an uninterrupted flow of blood from and to the apheresis machine. A blood bank employee prepares attaches a sterile, single-use tube set to the apheresis machine. This tube set is a closed system. Your blood is the only blood to flow through it, so you cannot contract an infection. Before the procedure commences the tube set is filled with salt water and anticoagulant (citrate); the tubes therefore contain no air. Approximately 250 ml of blood is present in the apheresis machine during the entire procedure. During the stem cell apheresis 15 liters of blood flow through the machine. An average of 50 to 70 ml of blood per minute flows from your body to the apheresis machine and back again. The procedure takes about 4 to 6 hours depending on the flow rate. The stem cell apheresis harvests only a few percent of your stem cell reserves.
Groin catheter
Sometimes the blood vessels in the arms are not suitable for connecting to the apheresis machine. The PA or internist hematologist then inserts a tube (catheter) in a blood vessel in the groin. This is done under a local anesthetic.
Because the groin catheter is placed in a large blood vessel, it is necessary to ensure sterile conditions. The doctor wears a mask, a sterile coat and gloves. The skin is sterilized with iodine where the groin catheter is inserted. The groin catheter is inserted under local anesthesia and takes about twenty minutes. Putting the materials ready requires some preparation time. The groin catheter has two openings, one for the outflow of the blood and one for the return of the blood. One catheter is therefore sufficient. The advantage of a groin catheter is that you can move your arms.
The groin catheter is removed one day after the stem cells have been harvested. This is because there is an increased risk of bleeding on the day of the stem cell apheresis. The groin is securely bandaged. You are not allowed to drive, but a designated driver or a taxi can drive you home. You must come back the next morning, driven by your designated driver or a taxi, to have the groin catheter removed.
Other possibilities
If harvesting fails, which happens only very rarely, there still is the option of obtaining the stem cells by means of several bone marrow punctures in both hips. These bone marrow punctures are performed under an anesthetic in an operating room.
Sometimes, in the interest of the patient, there can be a preference for stem cells obtained from the bone marrow. This is an entirely different procedure; no growth factors are used and no stem cell apheresis takes place.
If that is the case, it will be discussed with you. More information about this procedure can be found in the brochure entitled ‘Information for donors donating stem cells harvested from bone marrow’ and can be obtained from the SCT nurses.
Side effects of a stem cell apheresis
The following side effects may occur during stem cell apheresis:
Tingling
To prevent the blood from clotting in the apheresis machine, a blood thinning agent (citrate) is added. This thinning agent can bind calcium and thus reduce the calcium concentration in the blood. This can cause tingling in the hands, feet and around the mouth and sometimes cramp in the arms or legs. To prevent these symptoms, calcium is administered via the infusion, which is inserted by a nurse in the Hematology department. Should you nevertheless suffer complaints, it is important that you report them to the blood bank employee. You will then be administered more calcium via the infusion. You can also drink more milk or consume milk products on the day prior to harvesting the stem cells.
Bleeding tendency
The platelets can be damaged in the apheresis machine. After harvesting you might temporarily experience bruising or minor bleeding in the skin. Your blood counts are always checked immediately after the procedure ends. If the platelet count is too low, a transfusion with platelets might be necessary. This seldom happens with donors.
Discoloration of the urine
In rare instances, your urine can take on a slightly red color caused by red blood cells that were damaged in the apheresis machine. There is no need to worry. Your urine will be back to normal in about a day.
Fatigue
After enough stem cells have been harvested, you can return home. The long journey for some, fear of the unknown, the noise of the centrifuge, emotions and the changes in blood volume during the stem cell apheresis, cause most people to feel tired. We therefore advise you not to drive immediately after the procedure.
What is done with the harvested material?
The material is sent to the stem cell laboratory where the number of stem cells that have been harvested is determined (CD34+ determination). Sometimes it is necessary to harvest stem cells on a second day. 100 to 200 ml plasma is also collected during the stem cell procedure. The stem cell laboratory needs this plasma during the processing of the stem cells. Once enough stem cells have been harvested for transplantation the transplant is treated in the stem cell laboratory. The transplant consists of stem cells and T lymphocytes. The transplant usually contains some red blood cells. Depending on whether there is a difference in blood group between donor and patient, the transplant is treated so as to keep the number of red blood cells to a minimum.
During some treatments a number of T lymphocytes are taken from the transplant. Those T lymphocytes are frozen for possible later use in the course of the treatment.
The stem cell transplantation
The stem cells are ready to transplant the same day or the next day into the patient, your sibling. The stem cells are in an infusion bag and are administered similar to a blood transfusion.
The stem cells find their way via the bloodstream to the bone marrow where they implant themselves, multiply and stimulate the production of blood cells and the immune system. The chief physician and the nurse are present while the stem cells are being administered. You may also be present with your family member’s permission.
Aftercare
Outpatient appointments
After the stem cell apheresis you will have three aftercare appointments with the SCT nurse. The first appointment is a telephone consultation approximately 1 week after the apheresis. Two months and ten months after the apheresis it is necessary to have your blood checked, for which an appointment will be made for you with the SCT nurse.
Emotional aspects
Psychological stress
Of a completely different order, but certainly not something to be underestimated, is the emotional stress you might suffer from being asked to be a donor. Your family member gets the best available treatment; a decision made by the hematologic care team. But that doesn’t necessarily mean that the disease will simply go away and disappear. Your way of life, as a donor, has no influence on the patient’s healing process.
You most likely feel that you can help by donating stem cells. And rightly so. But later in the process you might suffer doubts or even guilt should complications occur with the patient or if the transplantation is unsuccessful. Should you feel the need to talk about this please do not hesitate to contact the SCT nurse.
Complications with the patient
The patient might possibly suffer the following complications after the stem cell transplantation:
- Graft-versus-host disease
It is possible that the donor’s white blood cells (the T lymphocytes) cause a severe immune response against the patient, the so-called graft-versus-host disease. This is the reverse rejection reaction. This disease can take a mild, severe or very severe course and it is possible that your sibling does not survive. It is not possible to predict whether a graft-versus-host disease can occur, nor how serious it will be. You, as a donor, have absolutely no influence on the development and course of this disease.
- Insufficient activity of the transplant
Sometimes the donor’s stem cells are not sufficiently active in the patient’s body. Only very occasionally, the donor’s stem cells can no longer be detected in the patient’s body. You, as a donor, have absolutely no influence on this either. We wish to stress that you, as a donor, can turn to us for any questions you may have, even quite a while after the transplantation has taken place. Please make an appointment for this with the SCT nurse. Or you can contact Hematon (www.hematon.nl), a contact group for patients, donors, family members and relatives. You will find a brochure about this in the hematology department.
Expenses/financial arrangements
If the patient is insured for medical expenses, all medical costs incurred by you, as a donor, are reimbursed by the patient’s health insurer. The G-CSF growth factor is provided by the pharmacy of the UMC Utrecht. Travel costs are reimbursed by your own health insurer. In this regard, you are to contact your health insurer yourself.
Absence from work in connection with stem cell donation is regulated in the ‘Dutch Payment of Wages during Illness Act’ (WULBZ)’. This regulation applies to disablement in connection with (stem cell) donation and pertains to the days on which you donate stem cells and any recovery period. Your employer reports you sick to employee insurance agency UWV during the stem cell donation day or days and your recovery period. Your employer can claim your paid wages from the industrial insurance board. Your absence in connection with the preliminary examinations is not covered by this regulation. Employers are free to contact the SCT nurse should they have any questions you cannot answer.
Naturally, we will never give them any confidential information such as results of your examinations or about the patient. If you are self-employed, you are entitled to a daily allowance if you have taken out voluntary disability insurance. You can contact your insurance company about this. If you are not insured, you will not be eligible for a daily allowance.
Canceling a holiday
If you have to cancel a holiday because of the stem cells procedure, you will not be able to claim your money back unless you took out cancellation insurance. If a medical certificate is required for your claim, it will be provided at the request of the insurer.
Cancer Center guest quarters
If you live far away, you and your partner or relative can stay overnight in the guest quarters. A charge applies to this accommodation. Depending on your insurance, this charge may or may not be reimbursed. You can reserve a room:
- By telephone on working days between 9 am and 4 pm; +31 (0)88 75 691 12;
- Via de website www.umcutrecht.nl/gastenverblijfcancercenter;
- Via e-mail gastenverblijfcancercenter@umcutrecht.nl;
- Or drop by the guest quarters at D3 east.
Additional treatment: Donor Lymphocytes Infusion (DLI) and Boost with stem cells
Donor Lymphocytes Infusion (DLI)
As part of being treated with an allogeneic stem cell transplantation it might be necessary at a later stage to give the patient more of the donor’s T lymphocytes. The donor’s T lymphocytes can influence the patient’s immune system.
Situations in which it is advisable to administer T lymphocytes to the patient are:
- Imminent failure of the transplant’s effectiveness;
- When a mixed image of patient and donor has developed in the bone marrow. Both the donor’s and the patient’s blood cells are produced. When the number of donor cells are in the minority or are decreasing, a donor lymphocyte infusion (DLI) can improve the situation;
- The (onset of a) relapse of the disease. If the disease returns very quickly, a DLI is usually no longer of any use;
- Insufficiently rapid recovery of the immune system;
- As part of the treatment for clinical studies: some of the T cells are frozen immediately after the stem cell apheresis.
In these cases you will be asked to undergo a second apheresis procedure. In this instance it is not necessary to inject a growth factor, considering there is no need to mobilize stem cells from the bone marrow. The matter here is the decrease of T lymphocytes, cells that under normal circumstances are present in the blood.
This apheresis procedure takes between 1 and 6 hours. If the patient is much heavier than the donor it is sometimes necessary to harvest T lymphocytes over the course of 2 days. After the apheresis, the number of cells is determined in the laboratory; the result is usually known within 30 minutes. The patient subsequently receives the cells via a peripheral infusion in the arm. This is usually done in an outpatient setting.
The main side effect of the DLI is the occurrence of the graft-versus-host disease, which can become apparent after 3 to 12 weeks. This side effect (see Chapter 10) is the result of a reaction of the donor’s T lymphocytes to the patient’s cells.
In some instances, there are grounds to repeat a DLI. Prior to the procedure for administering the donor lymphocytes, we ask you to sign another informed consent form.
Boost with stem cells
A stem cell boost can be given as soon as the transplant that was administered earlier is not responding adequately. During this procedure, stem cells, CD34+ cells, without immune cells, are returned to the patient. Your sibling’s hematologist will discuss with the treatment team whether there are any grounds for doing this procedure.
You will then be asked to undergo a second apheresis procedure. The procedure requires that the GCSF growth factor be injected to mobilize the stem cells from the bone marrow.
In conclusion
Planning
An allogeneic stem cell transplantation requires careful planning and coordination of all parties involved. The condition of the patient plays an important role as well. The date on which the transplantation will take place is known a number of weeks in advance. In connection with the afore-mentioned reason, this date cannot easily be changed. If you expect any important matters or occasions in your private life around that time or if you have planned a holiday, please notify us as soon as possible
Calamities
Some donors are afraid of catching a cold or becoming ill before the donation. Sometimes the people in your immediate surroundings will also keep a close eye on you. Of course you bear a certain responsibility, but you can live life, work and enjoy hobbies as usual. You can eat and drink as you normally would too. Only try to avoid unnecessary risks. Should you become ill, contact the SCT nurse as soon as possible.
Appendices
Glossary
Allogeneic
Originating from another individual.
Cytostatics
The collective noun for medicines that are used to treat cancer.
Erythrocytes
Red blood cells that transport oxygen.
Graft-versus-host disease
Immune response of the white blood cells of the donor cells against the patient.
Granulocytes
White blood cells that combat bacteria.
Leukocytes
White blood cells needed for the immune system.
Lymphocytes
White blood cells that respond to foreign invaders. T lymphocytes are cells that, after being transplanted, can cause a graft-versus-host disease.
Stem cell apheresis
The procedure for harvesting stem cells.
Stem cell mobilization
To ‘move’ the stem cells from the bone marrow to the circulating blood.
Thrombocytes
Small blood cells, ‘platelets’, which are necessary for hemostasis (stemming the flow of blood).
Frequently asked questions
How many liters of blood does a person have?
An adult person has a blood volume of approximately five liters. During stem cell apheresis, approximately fifteen liters of blood pass through the machine, so three times the blood volume.
Does a stem cell apheresis procedure always harvest sufficient stem cells?
It is not always possible to harvest the required number of stem cells in one apheresis procedure. Consequently, 2 consecutive days are always scheduled for harvesting.
Is the G-CSF always effective?
In exceptional cases, healthy people do not present enough stem cells in their blood while G-CSF is administered. In that case, you will be asked whether you are willing to donate bone marrow stem cells. Stem cells are harvested under anesthesia in the operating room by means of bone marrow punctures.
Can G-CSF be used during pregnancy?
Because not enough is known about whether G-CSF is safe for the unborn child and newborns, G-CSF should not be administered during pregnancy and breast-feeding. Women undergo a pregnancy test as part of the medical examination prior to the procedure. During the procedure female donors should take care not to become pregnant for up to 3 months after the G-CSF is administered.
Can one expect to suffer any side effects of G-CSF for any length of time after it has been administered?
G-CSF has been used since 1995 to mobilize stem cells for the treatment of patients. It has been administered in Europe to donors since 2001. There are no indications that serious side effects occur after a short-term treatment with G-CSF.
When do we know how many stem cells have been harvested?
A few hours after the stem cell apheresis is completed we will know how many cells have been harvested. It can then be said with certainty whether a second stem cell apheresis is required. If it turns out that a second stem cell apheresis is necessary, then G-CSF will also have to be injected.
What should I wear during the stem cell apheresis?
You will be lying down on a bed during the stem cell apheresis. Therefore, wear comfor- table, casual clothing, such as sweatpants and a T-shirt. Because of the infusion needles it is handy if you wear a short-sleeved shirt and possibly a cardigan over it.
Do I have to have an empty stomach on the day of the stem cell apheresis?
There is no need for you to fast. You may eat and drink as usual.
Important addresses and phone numbers
UMC Utrecht, Heidelberglaan 100
Postbus 85500
3508 GA Utrecht
The Netherlands
Hematology department, Location B2 east
+31 (0)88 75 576 55 Outpatients’ clinic (during office hours)
+31 (0)88 75 562 43/41 Nursing ward (after office hours)
Should you have any more questions, please contact the SCT nurse who is available on working days from 9:00 am to 4:30 pm.
Email: sctverpleegkundige@umcutrecht.nl
Telephone: +31 (0)88 75 736 27